The lymphatic drainage system of the breast plays a crucial role in immune function and detoxification, with superficial and deep lymphatics draining into axillary, internal thoracic, and supraclavicular nodes․
1․1 Overview of the Lymphatic System and Its Role in Breast Health
The lymphatic system, a network of vessels and nodes, plays a vital role in immune function and detoxification․ In breast health, it aids in removing toxins and proteins, supporting tissue health․ Superficial and deep lymphatics collaborate to ensure proper drainage, primarily through axillary nodes․ Understanding this system is crucial for managing breast cancer and preventing lymphedema, highlighting its importance in both health and disease․
1․2 Importance of Lymphatic Drainage in Breast Cancer Management
Lymphatic drainage is critical in breast cancer management, as it helps identify cancer spread through sentinel lymph node biopsies․ Proper drainage reduces lymphedema risk and enhances surgical outcomes․ Understanding lymphatic pathways aids in targeted therapies, minimizing complications and improving patient outcomes․ Effective lymphatic drainage strategies are essential for maintaining breast health and optimizing cancer treatment, ultimately contributing to better survival rates and quality of life for patients․

Anatomy of the Lymphatic Drainage System of the Breast
The breast’s lymphatic system includes superficial and deep vessels, with drainage primarily through axillary, internal thoracic, and supraclavicular nodes, forming interconnected pathways for lymph flow․
2․1 Superficial and Deep Lymphatic Vessels of the Breast
The breast contains both superficial and deep lymphatic vessels․ Superficial vessels are located near the skin, while deep vessels are embedded within the breast parenchyma․ These vessels play a critical role in immune response and detoxification by collecting lymph from breast tissue․ Superficial lymphatics primarily drain the skin, while deep lymphatics transport lymph from the glandular tissue․ Together, they form an intricate network ensuring efficient lymph circulation․
2․2 Axillary, Internal Thoracic, and Supraclavicular Lymph Nodes
Axillary lymph nodes are the primary drainage sites for the breast, located in the armpit․ Internal thoracic nodes are situated behind the sternum, while supraclavicular nodes are above the collarbone․ These nodes filter lymph from the breast, detecting pathogens and cancer cells․ Their arrangement and function are vital for diagnosing and managing breast cancer, influencing treatment strategies and patient outcomes significantly․
Physiology of Breast Lymphatic Drainage
Breast lymphatic drainage involves lymphatic capillaries collecting fluid from lobules, flowing into axillary and internal thoracic nodes․ Manual techniques enhance this process, aiding detoxification and immune function;
3․1 Mechanisms of Lymph Flow and Drainage Patterns
Lymphatic capillaries in the breast lobules collect fluid, which flows through intramammary nodes into axillary and internal thoracic pathways․ Pressure gradients and intrinsic contractions propel lymph upward․ Manual techniques enhance this process, ensuring efficient detoxification and immune support․ Drainage patterns vary, but axillary nodes are the primary route for breast lymph․ This mechanism is vital for maintaining breast health and preventing lymphedema․
3․2 Role of Intra-Mammary Lymph Nodes in Breast Drainage
Intra-mammary lymph nodes, located within the breast parenchyma, act as intermediaries in lymphatic drainage․ They filter lymph from lobules and ducts before redirecting it to axillary or internal thoracic nodes․ These nodes are crucial for detecting pathogens and abnormal cells, playing a key role in both immune defense and cancer detection․ Their strategic location ensures efficient lymphatic circulation, maintaining breast health and facilitating early disease diagnosis․
Clinical Relevance of Breast Lymphatic Drainage
Breast lymphatic drainage is vital in cancer management, influencing sentinel lymph node biopsy, lymphedema prevention, and treatment planning․ Understanding these pathways enhances personalized therapy and reduces complications․
4․1 Sentinel Lymph Node Biopsy and Its Implications
Sentinel lymph node biopsy is a critical diagnostic tool in breast cancer, identifying the first nodes receiving lymphatic drainage from the tumor․ Accurate mapping ensures precise staging, guiding treatment decisions and minimizing unnecessary lymph node removal․ This procedure reduces complications like lymphedema, emphasizing the importance of lymphatic anatomy in modern breast cancer management and patient outcomes․
4․2 Lymphatic Drainage in Breast Cancer-Related Lymphedema
Lymphatic drainage dysfunction is a key factor in breast cancer-related lymphedema, where impaired flow leads to fluid accumulation․ Techniques like MLD and Kinesio-Taping help restore lymphatic circulation, reducing swelling and enhancing comfort․ Early intervention is crucial to prevent progression, emphasizing the role of lymphatic drainage in both prevention and management of lymphedema, improving quality of life for breast cancer survivors․
Manual Lymphatic Drainage (MLD) Techniques for the Breast
Manual Lymphatic Drainage (MLD) is a gentle therapy used to promote lymph flow, reducing swelling and enhancing breast health․ Techniques involve light, rhythmic strokes to stimulate lymph nodes and vessels, encouraging fluid drainage and supporting detoxification․
5․1 Step-by-Step MLD Massage Techniques for Breast Health
Begin with light pressure, massaging the axilla to stimulate lymph nodes․ Use gentle, rhythmic strokes toward the collarbone to aid lymphatic flow․ Focus on the breast tissue, applying soft, circular motions to promote drainage․ Ensure strokes follow the natural direction of lymph flow․ Finish with deep, calming breaths to enhance relaxation and lymphatic circulation․ Always maintain gentle pressure to avoid discomfort․
5;2 Benefits and Contraindications of MLD in Breast Care
MLD enhances lymphatic circulation, reducing swelling and promoting healing․ It alleviates lymphedema and improves breast health post-surgery․ However, contraindications include active cancer, infections, or acute inflammation․ Patients with heart conditions or implanted devices should avoid MLD․ It is also contraindicated in severe kidney or liver dysfunction and during pregnancy․ Consultation with a healthcare professional is essential before starting MLD therapy․
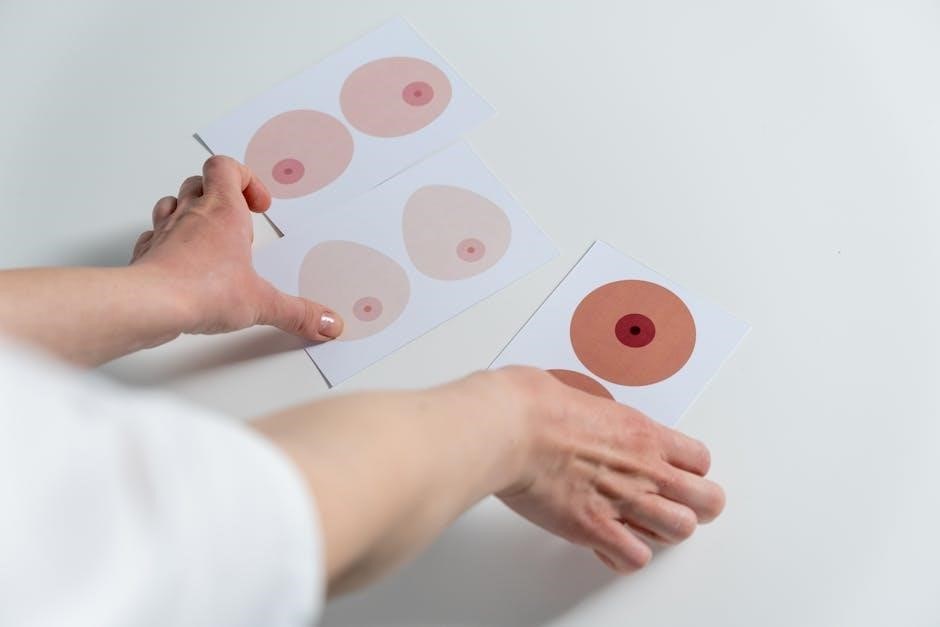
Imaging of Breast Lymphatic Drainage
Imaging techniques like lymphoscintigraphy and ultrasound are essential for visualizing lymphatic pathways and nodes, aiding in accurate diagnosis and treatment planning for breast-related lymphatic conditions․
6․1 Role of Imaging in Assessing Lymphatic Anatomy
Imaging techniques such as lymphoscintigraphy and ultrasound play a vital role in mapping lymphatic pathways and identifying nodes․ These methods provide detailed visualization of lymphatic vessels, aiding in the assessment of drainage patterns and anatomical variations․ Accurate imaging helps diagnose lymphatic dysfunction and guides interventions, particularly in breast cancer and lymphedema cases, ensuring precise clinical decision-making and treatment planning․
6․2 Lymphoscintigraphy and Ultrasound in Lymph Node Mapping
Lymphoscintigraphy uses radioactive tracers to visualize lymphatic pathways, while ultrasound provides real-time imaging of lymph nodes․ Together, these techniques enhance the accuracy of lymph node mapping, aiding in sentinel lymph node identification and cancer staging․ They are particularly valuable in breast cancer management, offering complementary insights into lymphatic anatomy and function, thereby improving diagnostic precision and treatment planning․

Extra-Axillary Lymphatic Drainage Pathways
Breast lymphatic drainage extends beyond the axilla, with pathways to internal thoracic and supraclavicular nodes․ These routes are critical for comprehensive lymphatic circulation and cancer management strategies․
7․1 Internal Thoracic and Supraclavicular Lymphatic Pathways
The internal thoracic lymphatic pathway drains the medial aspect of the breast, while the supraclavicular pathway serves as an alternative route for lymphatic flow․ These pathways are critical for ensuring proper lymph circulation, especially in cases where axillary nodes are compromised․ They play a significant role in breast cancer management and lymphedema prevention, offering additional drainage routes for lymph fluid․
7․2 Clinical Implications of Extra-Axillary Drainage
Extra-axillary drainage pathways, including internal thoracic and supraclavicular routes, significantly impact breast cancer management․ They provide alternative lymphatic flow when axillary nodes are removed or blocked․ Understanding these pathways aids in precise sentinel lymph node biopsies and reduces lymphedema risk․ Accurate mapping of these routes enhances treatment planning and improves patient outcomes in breast cancer care and lymphatic system rehabilitation․

Prevention and Management of Lymphedema
Preventing lymphedema involves early detection, manual lymphatic drainage, controlled exercises, and compression garments․ These strategies reduce swelling and improve lymphatic flow, enhancing overall breast health and patient well-being․
8․1 Role of Lymphatic Drainage in Lymphedema Prevention
Lymphatic drainage plays a pivotal role in lymphedema prevention by promoting the removal of excess fluids and proteins from breast tissues․ Manual lymphatic drainage (MLD) techniques, such as gentle massage targeting the axilla and supraclavicular nodes, stimulate lymph node activity, enhancing circulation and reducing swelling․ Regular practice of these methods can significantly lower the risk of developing lymphedema, especially in patients with compromised lymphatic systems․
8․2 Combined Therapies for Lymphedema Management
Combined therapies, such as manual lymphatic drainage (MLD), Kinesio-taping, compression garments, and exercises, are essential for lymphedema management․ These methods enhance lymph flow, reduce swelling, and improve tissue elasticity․ MLD stimulates lymph node activity, while compression garments provide sustained pressure to prevent fluid accumulation․ Regular exercise strengthens muscles, aiding lymph circulation․ Together, these therapies offer a holistic approach to managing lymphedema effectively․
Modern Techniques in Breast Lymphatic Drainage
Modern techniques in breast lymphatic drainage include Kinesio-taping and microsurgical lymphatic reconstruction, aiding in efficient lymph flow, reducing swelling, enhancing circulation, and minimizing discomfort for optimal breast health․
9;1 Lymphatic Reconstruction and Microsurgical Techniques
Lymphatic reconstruction and microsurgical techniques are advanced methods to restore lymphatic pathways, preventing lymphedema and enhancing drainage․ These procedures involve precise surgical interventions to reconnect or bypass damaged lymphatic vessels, improving circulation and reducing swelling․ Microsurgery is particularly effective in breast cancer patients, offering a minimally invasive approach to restore lymphatic function and improve overall recovery outcomes․ These techniques are pivotal in modern breast lymphatic drainage management․
9․2 Kinesio-Taping and Its Role in Lymphatic Drainage
Kinesio-Taping is a non-invasive technique that supports lymphatic drainage by applying gentle pressure to the skin, enhancing the flow of lymph fluid․ It is particularly beneficial for patients with breast cancer-related lymphedema, as it helps reduce swelling and promote circulation․ Studies show that Kinesio-Taping, when combined with manual lymphatic drainage, significantly improves lymphatic function and patient comfort, making it a valuable adjunctive therapy in breast lymphatic care․
10․1 Summary of Key Concepts
Lymphatic drainage of the breast is essential for immune function and detoxification, with pathways involving axillary, internal thoracic, and supraclavicular nodes․ Understanding its anatomy and physiology aids in breast cancer management, lymphedema prevention, and sentinel lymph node biopsies․ Techniques like manual lymphatic drainage and imaging modalities enhance diagnosis and treatment․ Future research focuses on innovative therapies and lymphatic reconstruction to improve patient outcomes and quality of life․
10․2 Emerging Research and Innovations in Breast Lymphatic Drainage
Emerging research explores nanotechnology for targeted lymphatic therapy, advanced imaging for precise node mapping, and microsurgical techniques to restore lymphatic pathways․ Innovations like wearable devices and bioengineered scaffolds aim to enhance lymphatic function․ Personalized medicine approaches, including genetic profiling, are being investigated to optimize treatments for lymphedema and breast cancer management, promising improved outcomes and reduced complications․